It is important to learn about postpartum mood and anxiety disorders because knowledge is often the best defense. Our society, unfortunately, still stigmatizes these experiences, causing new parents to be afraid to talk about them and seek help.
This quote comes to mind:
…there are two ways of going about liberation: one, of course, is the political way, changing the laws and fighting for equalities… But the other I stress simply because it is the one I know: the psychological way, which is the removal of obstacles so that you can create your own freedom and you don’t have to ask for it. You don’t have to wait for it to be given to you. And the women I chose as my heroines were women who created their own freedom. They didn’t demand it, they didn’t ask for it. They created it. It is very easy to blame society… but it actually makes you feel even more helpless. Because that means you are waiting for [society] to liberate you, for the government to liberate you or for history. And that takes a long time. It takes centuries, and that is too slow for me. We only have one life.
Anais Nin
This quote may be referring to women’s equality, but I feel it fits with what stands in the way of families getting help. Certainly, the stigma isn’t the only barrier, but it is a big one. So what if parents stood up and felt they could get help without self-judgment or judgment from others? Our own self-judgment is something we can control and that is all that matters, really.
What you might not know is that postpartum mood and anxiety disorders can be prevented or at least minimized.
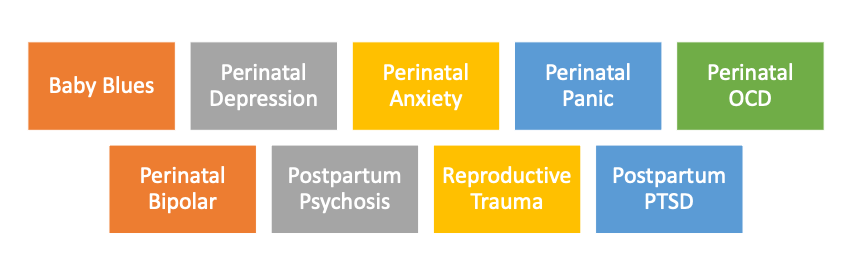
First, I need to shift some language. Yes, the term “postpartum mood and anxiety disorders” is correct, but describes a shorter window. Perinatal mood and anxiety disorders can affect parents at any time -during pregnancy, during the first year after delivery, during the first year after a perinatal loss, during the first six months after weaning from breastfeeding, and even after the first year after delivery.
So how can a perinatal mood and anxiety disorder be prevented or at least minimized?
Understanding what the risk factors are, what the symptoms look like, and how to get help, is the best line of defense. And you also need to understand what is included in perinatal mood and anxiety disorders (PMADS):
Baby Blues
Baby blues impact about 80% of women and can last for 2 to 4 weeks after delivery. It typically occurs within 10 days after delivery with symptoms that include crying spells, feeling overwhelmed, and feeling down. This experience is brief and doesn’t require intervention. But that doesn’t mean you don’t need emotional support from your support system. However, if these symptoms persist after 4 weeks, then it is considered postpartum depression.
Perinatal Depression (but most people think of this as just postpartum depression)
Perinatal depression impacts 1 in 5 women, 1 in 3 women of color, and 1 in 10 dads.
Again, 1 in 3 new mothers of color experience a perinatal mood and anxiety disorder. This is twice the rate of white women. Genetic differences are not the reason women of color experience a PMAD at a higher rate than white women.
Socioeconomic status and systemic racism are some reasons why WOC are at a higher risk and why WOC are less likely to receive treatment.
Treatment providers are still predominately white and lack an understanding of multicultural differences. But there are still differences in how WOC are treated in the health care system compared to white women.
There are also epigenetic reasons like chronic stress as a result of transgenerational trauma putting WOC at a higher risk for a perinatal mood and anxiety disorder.
Symptoms of perinatal depression include:
- Feeling down
- Loss of interest in things you previously were interested in
- Sleep disturbances
- Increased or decreased weight
- Difficulty concentrating
- Fatigue
- Frustration
- Grief
- Anxiety – the hallmark symptom of perinatal depression
- Anger/rage
- Inappropriate guilt
- Feeling disconnected from the baby
- Difficulty caring for the baby
- Suicidal ideation
Remember that you are reading this because understanding what the risk factors are, what the symptoms look like, and how to get help, is the best line of defense.
Perinatal depression is the #1 complication of childbirth
Perinatal Anxiety Disorders
Symptoms of anxiety are very common in the perinatal period and can present alone or with depression.
Symptoms of perinatal anxiety include:
- Hypervigilant concerns about something happening to you or the baby
- Difficulty sleeping when the baby is sleeping
- Irritability
- Appetite changes
- Racing thoughts
- Physical symptoms such as shortness of breath, heart palpitations, digestive issues
Perinatal Panic Disorder
This is a more severe version of perinatal anxiety. The 3 common fears associated with perinatal panic are fear of losing control, fear of losing your mind, and fear of dying.
Perinatal panic symptoms include:
- Episodes of extreme anxiety
- Excessive worry or fear
- Panic either keeps the parent awake or suddenly wakes the parent up
- Restlessness leading to irritability
- More physical sensations; hot or cold flashes, tingling, trembling, or numbness
- Fear of having a panic attack
- Generalized anxiety
- Can lead to agoraphobia
Perinatal Obsessive Compulsive Disorder
There are two types of presentations with perinatal obsessive-compulsive disorder. One is having intrusive and scary thoughts that can include the parent harming the baby which can lead to fear of carrying out the thoughts. These thoughts are ego-dystonic which means, they are horrifying to the parent and inconsistent with their value system.
So know that if you have intrusive thoughts that scare you, you are not in danger of harming your baby.
The other is under traditional OCD obsessions and compulsions related to contamination.
Symptoms of perinatal OCD include:
- Intrusive, repetitive thoughts-usually of harm coming to the baby, or parent harming the baby
- Tremendous guilt and shame
- Horrified by these thoughts
- Hypervigilance
- Checking online
- Parent engages in behaviors to avoid or minimize obsessions or intrusive thoughts
Remember that you are reading this because understanding what the risk factors are, what the symptoms look like, and how to get help, is the best line of defense.
Perinatal Bipolar Disorder
Bipolar I
It consists of alternating periods of severe depression and elevated mood (hypomania or mania). If a diagnosis of bipolar disorder has been given and medication has been discontinued during pregnancy, there is a 71% rate of relapse before the end of pregnancy. Because a woman can have her first manic episode in the postpartum period, she may initially be prescribed an antidepressant. Since 60% of bipolar women initially present as depressed, an antidepressant alone can cause her to cycle into her first manic episode. People diagnosed with bipolar disorder have depression that is resistant to therapy and can respond poorly to medication.
Elevated mood symptoms include:
- Euphoria or agitation
- Decreased need for sleep
- Racing thoughts
- Increased productivity noticed by others
- Pressured speech
- Increased energy
- Anxiety
- Rage
- High-risk behaviors
Another sobering fact is, 50% of women with bipolar are 1st diagnosed in the postpartum period.
Bipolar disorder is closely related to postpartum psychosis. Statistically, 1 out of 50 women with a bipolar diagnosis may develop postpartum psychosis. This is a period of heightened vulnerability, so early intervention is important to avoid a psychiatric emergency. Early intervention can include making sure you are taking your medication and your medication is being managed by a reproductive psychiatrist or a physician who understands bipolar and the perinatal period. Another early intervention would be to see a therapist who specializes in perinatal mental health. Finally, make sure your support system understands postpartum psychosis, what to look out for, and who to contact in an emergency.
Bipolar II
Bipolar II may not cause any impairment in functioning but the symptoms include:
- Moodiness
- Irritability
- Rage
- Anxiety
- Insomnia
- Hypomanic episodes may last 1-6 days
The hypomanic phase can develop immediately after delivery with severe depression occurring several weeks later.
Remember that you are reading this because understanding what the risk factors are, what the symptoms look like, and how to get help, is the best line of defense.
Postpartum Psychosis
Postpartum psychosis is rare, occurring in 1 – 2% of all postpartum women. It can occur 3 to 14 days after delivery with symptoms coming and going.
The symptoms include:
- Irrational and incoherent statements
- Extreme confusion
- Severe agitation
- Thoughts of harming self or baby based on delusional thoughts or hallucinations
- A loss of touch with reality
The delusions or hallucinations are typically religious in nature with fear that the devil is trying to possess the baby, the baby is the devil, or something terrible is destined to happen to the baby. This is where there is an elevated risk for suicide and or infanticide. Thoughts of harming her baby are ego-syntonic which means the mother thinks or believes she is protecting her baby and acting reasonably or rationally – but she does NOT desire to harm her baby.
I want to emphasize that an elevated risk does not mean any woman who experiences postpartum psychosis will automatically harm her baby, but it is considered an emergency so it is important to know that there are mother-baby hospitals that provide support and treatment for moms while still being able to maintain connection and attachment with her baby.
If that is not an option, Postpartum Support International has resources by state and some countries that you can call to find help.
Risk factors for postpartum psychosis are:
- Personal history and family history of psychosis
- A diagnosis of bipolar
- A diagnosis of schizophrenia
- A diagnosis of schizoaffective disorder
Other factors that can contribute are:
- Hormone shifts
- OB complications
- High environmental stress
- Sleep deprivation – 3 days without sleep can cause a psychotic episode
Remember that you are reading this because understanding what the risk factors are, what the symptoms look like, and how to get help, is the best line of defense.
Reproductive Trauma
Reproductive trauma includes difficulty getting pregnant or having to go through IVF, miscarriage, stillbirth, loss in multifetal pregnancy, or elected termination. When a parent experiences any of these situations, there is loss. It can also be called traumatic grief.
It is different than losing a parent because a parent is a part of your past, but a baby is a part of your future and a part of your identity. Reproductive trauma doesn’t just impact the person carrying the baby, it impacts the whole family – siblings, parents, grandparents, and even aunts and uncles.
When there is a loss, there are always reminders, like the due date of the baby, and every year after on that day, going to baby showers, family members or friends who are pregnant or delivering at the same time your baby was to be born, the nursery that has been set up, or if the loss is recent, you still have a baby bump, and people ask when you are due.
Postpartum PTSD
Postpartum PTSD can be a response to perinatal loss, but it is also a response to a traumatic experience during pregnancy, a traumatic experience while giving birth (birth trauma), or a traumatic experience post-birth.
Birth Trauma
“In the beginning of my research traumatic childbirth was viewed as an event that occurs during labor and delivery that involved actual or threatened serious injury or death to the mother and or her infant. After my first 2 studies on birth trauma and its resulting PTSD what I learned was that traumatic childbirth can also occur even if a woman does not perceive that she or her infant is at risk for serious injury or death. Women can perceive their birth as traumatic if they perceive that they were stripped of their dignity during the birthing process.”
Cheryl Tatano Beck DNSc, CNM
Many birth parents have an idea of what they want the birth to look like and have a birth plan. It can also be traumatic if the birth didn’t turn out the way they wanted or expected.
Post-birth Trauma
Post-birth trauma occurs when there are medical complications with the mom after delivery, neonatal complications, or the baby in the NICU. And these are all terrifying and traumatic experiences.
Symptoms of postpartum PTSD are:
- Re-experiencing trauma (flashbacks)
- Avoidance/numbing of aftercare
- Poor concentration
- Sleep disturbance
- Impaired mother-infant bonding
- Sexual dysfunction
- Increased anxiety/arousal
- Avoidance of reminders of childbirth
- Pre-occupation with memories of childbirth
Remember that you are reading this because understanding what the risk factors are, what the symptoms look like, and how to get help, is the best line of defense.
Possible Risk Factors:
- Family history of depression and anxiety, including PMAD
- Personal history of depression, anxiety, OCD
- Having multiples
- Inadequate support (family, social, financial)
- ADHD
- Single mothers
- Teen mothers
- Reproductive trauma (infertility, perinatal loss, elected termination, birth trauma)
- Major life transition (moving, new job, deployment)
- Complicated pregnancy
- Difficulty breastfeeding
- Abrupt discontinuation of breastfeeding
- Sensitive to hormone shifts
- History of PMDD (Premenstrual Dysphoric Disorder)
- Endocrine disorders such as hyper/hypothyroidism or other reproductive conditions
- Highly sensitive person (HSP)
- Barriers to support, including systemic racism
- Intimate partner violence
- History of sexual, physical, and/or emotional abuse as a child
- Lack of compassion or inappropriate and unprofessional comments from medical staff before, during, or after delivery
- Believing the myths of parenthood
So what are some myths about parenthood?
- There is such a thing as a perfect mother/father/parent
- Parents are supposed to self-sacrifice for their children
- Breastfeeding is easy
- If you don’t breastfeed, you aren’t a good mother
- Parenthood is the happiest time in your life
- Perinatal depression is only experienced by a woman who has given birth
- All parents experiencing perinatal depression look depressed
- Depression is the only symptom of perinatal depression
- The onset of perinatal depression is only a few weeks after delivery
- Parents automatically know what their baby wants and needs by instinct
There may be some myths you received growing up about parenthood that impact how you think you are supposed to be in order to take care of and love your child. Take some time and get curious about those messages. Ask yourself if these belief systems match your value system, or benefit your mental health.
I know this is a heavy topic and a lot of information to take in. And you are probably asking yourself, what am I supposed to do with all of this information?
First, I want you to breathe. You might be overwhelmed. If you are, put the information away, go for a walk, or do anything else you do to help calm yourself. Then, take some time to just process it. There is no rush. Once you have had time to process it, take inventory of your risk factors.
Write down who is in your support system – your village. Your support system is probably THE most important part of prevention or minimization. If you are taking medication that benefits your mental health, talk to your doctor about staying on it. Find a therapist who understands perinatal mental health and get started to discuss ways to feel supported during this time.
Remember you read this because understanding what the risk factors are, what the symptoms look like, and how to get help, is the best line of defense. And reading this to help take care of yourself proves that you are going to be or are a good parent.
Jacqueline V. Cohen is a licensed professional counselor and an ADHD-certified clinical specialist provider specializing in perinatal mental health and adult ADHD. To learn more about her services, you can go to her website. You can also contact her by email.
Get your free copy of my e-book: Motherhood and ADHD
You will also receive a subscription to my newsletter.



